#Allergies, the Immune System and your Microbiome
An estimated 50 million Americans suffer from allergies, which occur when the immune system becomes hypersensitive and reacts against otherwise harmless substances. In my last post I discussed how the best solution is to never become allergic in the first place. But early childhood seems to be key there, and for many adult allergy sufferers, it’s too late. So what can one do to help alleviate suffering from allergies?
##Air-borne Allergens and Asthma
Multiple sources point to sensitivity to air-borne allergens being driven, at least in part, by interactions with the microbiome. This can be either the microbiome of the lungs (Gollwitzer et al., 2014) or the microbiome of the gut (Trompette et al., 2014).
###Microbial diversity and asthma Huang et al. (2011) did a clinical study that showed some light on the relationship between microbial diversity and asthma (part of a trial trying to understand why therapy with certain antibiotics, macrolides, seems to improve pulmonary function on Asthma patients) . They collected samples from the bronchia of 65 adults with sub-optimally controlled asthma who were undergoing an antibiotic therapy, as well as a control group of 10 healthy individuals. The asthmatic samples tended to have higher concentrations of microbes. They also tended to have higher diversity of microbes than their healthy counterparts. Now, this is where this study gets tricky: The people that responded to antibiotic therapy had higher diversity of microbes than the people that didn’t respond to therapy.
Wait, what???
Yeah, that’s exactly what I thought myself. So, let’s try to make sense of it:
- Airway Microbial Diversity low -> healthy
- Airway Microbial Diversity medium -> asthma + not responding to therapy
- Airway Microbial Diversity high -> asthma + yes responding to therapy
This is an unexpected result, since usually what we see is a gradient of negative effects that gets smaller as it gets closer to a “healthy configuration.”
In multivariate analyses airway microbiota composition and diversity were significantly correlated with bronchial hyperresponsiveness. Specifically, the relative abundance of particular microbial phylotypes, including members of the Comamonadaceae, Sphingomonadaceae, Oxalobacteraceae, and other bacterial families were highly correlated with the degree of bronchial hyperresponsiveness.
One thing that might be limiting the usefulness this study is the limited number of patients. They start with 65, which is already a small cohort, but the relationship between pre-treatment diversity and response to treatment is drawn only from 12 patients (3 did not respond, 9 responded to treatment). These are fairly small numbers, and sometimes when one is doing a study, it’s hard to get more human samples, so you work with what you have, and hope that you shed enough light for somebody after you to do a better job.
###Your microbiome is more than just bacteria Also, when you thought things were complicated enough, there comes another wrinkle. Most of the things we have been talking so far are about bacteria. But, it happens that the lungs have fungi too. In fact, when you look at the fungi, the ones in asthma patients vs. the ones in health controls, guess what? They are different (van Woerden et al., 2013). The figure below shows the change in fungi between asthma (red) and control (blue).
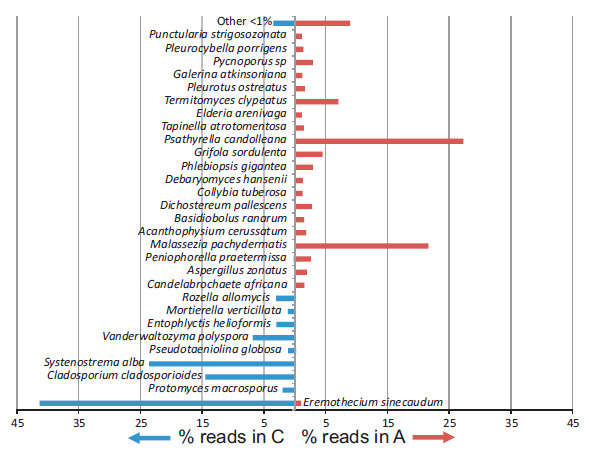
From van Woerden et al., 2013
Graph showing the percentage of pyrosequencing reads for fungal species identified in the Asthma patient (A) or control participant (C) samples (species unidentified for reads greater than 1%). van Woerden et al.; BMC Infect Dis. 2013 Feb 5;13:69. doi: 10.1186/1471-2334-13-69. Differences in fungi present in induced sputum samples from asthma patients and non-atopic controls: a community based case control study. This image is under Creative Commons Attribution License, original source at http://www.biomedcentral.com/1471-2334/13/69.
This suggests that this whole problem needs an additional look, since fungi can be as, or perhaps even more important than bacteria for some scenarios.
##Food Allergies and Food Intolerances
Little research has been done linking specific serious food allergies to the microbiome. If you have been diagnosed with a food allergy because of prior anaphylaxis or clinical diagnosis, be certain to follow the medical guidance you’ve received and do not expect probiotic supplements to cure or alleviate this allergy.
That said, people often casually refer to foods that have proven in the past difficult to digest as foods they are “allergic to.” Often these digestive challenges may be a sign of a weakened digestive system: see our Home page for more information about your gut flora and how you might experience evolutionary normal digestion.
##Allergy Treatment Allergy treatment has been evolving quickly in recent years. Currently, avoidance of exposure to allergens and preparation to treat any emergency (sometimes including medicines like cetirizine and injectable epinephrine) is the recommended approach (Sicherer and Sampson, 2014).
For adults, a promising avenue is Treg therapy: that is, therapy based on regulatory T cells (Tregs) (reviewed in Wright et al., 2011), but it is still in its early stages of development. One of the most promising avenues is the Inflammation/Sepsis model, based on a study using mice (Heuer et al., 2005). Their results suggest that Treg therapy can improve the outcome for a mouse model of sepsis. Specifically, mice that were subject to stimulated Tregs had significantly improved survival. Their results suggest a novel role for Tregs in sepsis.
Additional mouse studies studies show specific probiotic treatments resulting in a Treg increase along with decreased airway reactivity: L.rhamnosus GG and Bifidobacterium lactis (Bb-12) (Felezko et al., 2007); L. salivarius and L. reuteri (Karimi et al., 2009). Just remember that often times, results in animal models do not translate to humans.
Allergy treatment will continue to evolve as scientists learn more. As we improve our understanding, perhaps humankind might escape from some of the suffering that allegies cause.
Reminder: This is a tour of the scientific literature, not medical advice or an alternative to the opinion of your doctor. Please behave responsibly and use it for intellectual appreciation, not self-treatment.
Sign post: For an overview of Equilibrium’s design, please see the product page and scroll down. We also welcome questions at questions@generalbiotics.com.